What is DADA2?
DADA2 is a rare, monogenic recessively inherited autoinflammatory disease characterized by systemic inflammation, vasculitis, early-onset stroke, immunodeficiency, and bone marrow failure. The first signs of the disease can be chronic and mild, or severe and acute such as an early onset stroke.
Approximately 25% of patients are diagnosed before one year of age and 77% by 10 years of age. Patients with DADA2 who have bone marrow failure tend to present during early infancy, whereas delayed presentation is common in patients with vasculitis affecting medium- and small-sized vessels and systemic inflammation. The mortality is estimated at approximately 8% before the age of 30.
While we only know of approximately 600+ DADA2 patients today, a 2021 study with the DADA2 Foundation, Boston Children's Hospital, and the Broad Institute, suggests 35,000 patients could be affected and undiagnosed globally.
Early diagnosis is critical to minimize systemic organ damage. The best treatments today are TNF inhibitors for the autoinflammatory aspects of the disease. TNF inhibitors have been shown in retrospective clinical studies to reduce autoinflammation and in patients who have had strokes, prevent strokes from recurring. For those with critical bone marrow failure, a bone marrow transplant may be necessary.
The clinical spectrum of DADA2 is broad, and manifestations can vary even among family members with the same genotype.

When was DADA2 Discovered?
For decades, the science around ADA2 – adenosine deaminase 2 – trickled out slowly. Despite some research, the enzyme’s function in humans remained elusive. Meanwhile, patients suffered with severe and debilitating symptoms from recurring fevers, vasculitis and pain, to life-altering strokes and bone marrow failure.
The disease itself was finally discovered in 2014 and published in the New England Journal of Medicine (NEJM) by two independent groups at the National Institutes of Health (NIH) and in Jerusalem, Israel, each reporting systemic inflammation and vasculitis caused by mutations in the ADA2 gene. After the publications, a small group met in Houston, Texas at the Clinical Immunology Society meeting to discuss planning a DADA2 conference, with an inaugural conference occurring in 2016. The collaboration at that meeting set off a record-fast pace of clinical and scientific work.
What are the Signs & Symptoms of DADA2?
Meet the DADA2 Human Interactive Graphic
Signs & Symptoms
Click on an organ name to get clinical information about signs & symptoms of DADA2.
Diagnosing DADA2
Before being tested for DADA2, many patients remain undiagnosed for years, suffering some combination of debilitating pain, fatigue, fevers, rashes, organ damage due to vasculitis and systemic inflammation, severe anemia or other cytopenias, and recurrent strokes.
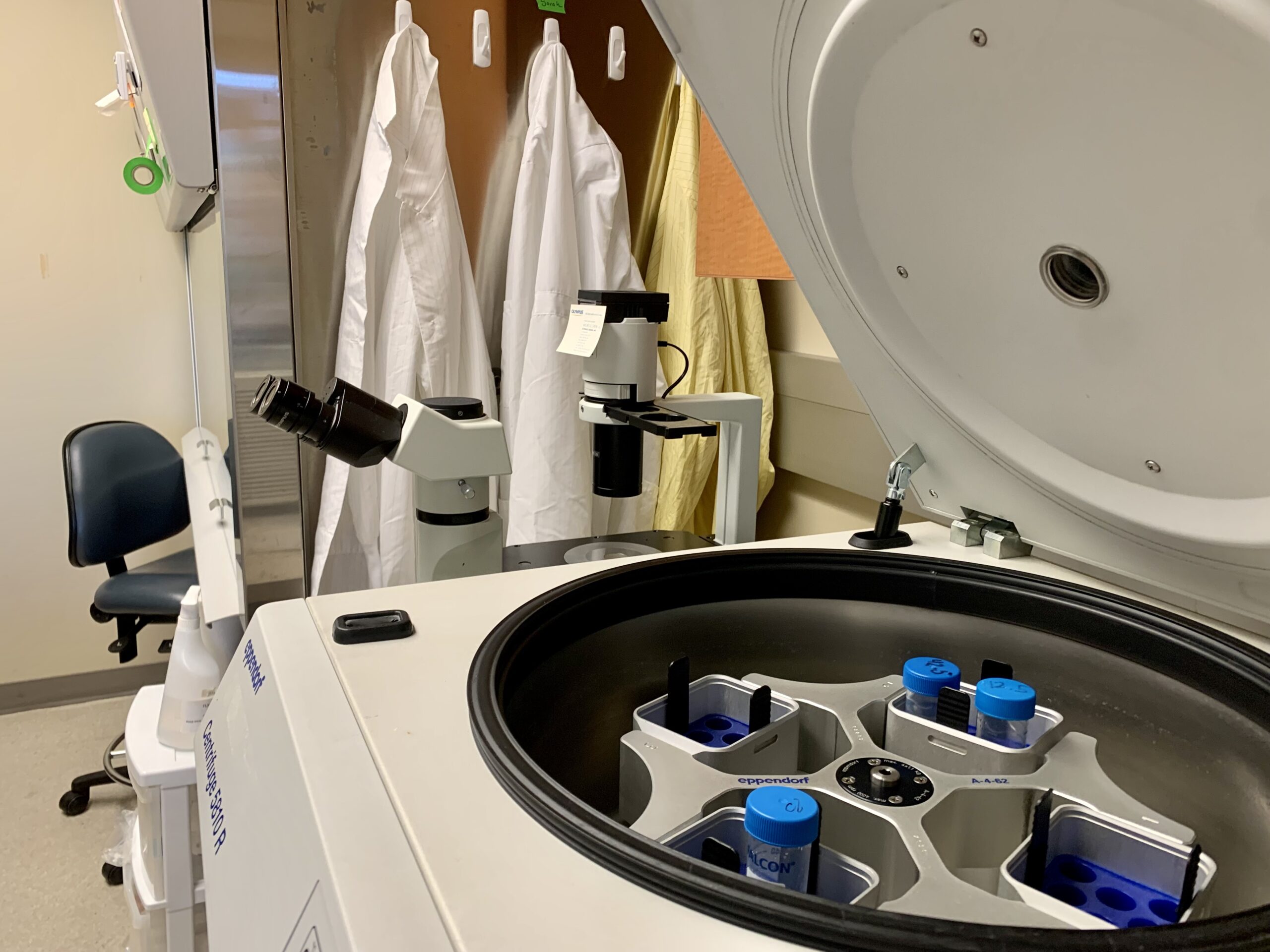
Diagnosing DADA2 can be tricky since symptoms can mimic so many other diseases. After a good history and physical exam that may suggest a diagnosis of DADA2, it is diagnosed by genetic sequencing and/or ADA2 enzyme activity testing. A blood draw is the usual method for both tests.
A deep dive into Deficiency of Adenosine Deaminase 2 - its causes, diagnosis, treatment, and future prospects with leading pediatric rheumatologist Dr. Pui Y. Lee.